By: Jaclyn Rink, MSCP, LLP
You’ve probably heard someone say the following “Ugh! Sorry! I am SO OCD about that!” In our everyday language, people often use this phrase as a way to highlight frustrations with cleanliness perfectionism, or uniformity. Truth is, obsessive compulsive disorder is not an adjective, it’s a noun. Therefore, we cannot use it to describe an eccentricity, personality trait, or personal preference. Instead, we need to remember that it is a serious mental condition that affects 2% of the population (one out of every 40 people) at some point in their lifetime. OCD is often chronic, causing ongoing frustration and impairment in individuals, and it is much more intense and complex than a quirky characteristic. It has to potential to cause emotional, social, academic, vocational, and even physical distress, often interfering with a person’s day-to-day functioning.
Doesn’t seem so simple, huh? How much do you really know about OCD? After working closely with OCD patients for the past 8 years, here are some of the biggest misconceptions, clarified:
1. OCD is just all about germs and washing your hands: OCD is way more than just germs! In fact, it has several subcategories. People with OCD can present with any of the following obsessions or compulsions (jointly or individually):
-Contamination and germs
-Symmetry and order
-Harm OCD (to oneself and others)
-Checking (incompleteness and self-doubt)
-Sin, religion, and morality
-Hoarding
-Aggressive or sexual thoughts
Ex: The person that is STILL apologizing for and thinking about a mistake they made 5 years ago? Morality
Ex: Your child asks you 6 times in a row if you love them, despite a consistent answer? Checking.
Ex: The man who won’t drive on the freeway because they don’t trust themselves at high speeds? Harm.
Ex: The woman you know that takes 4 hours to get ready in the morning because she cleans up the bathroom after her shower? Contamination.
2. You can tell if someone has OCD: Mainstream media leads us to believe that the compulsions that accompany intrusive thoughts are all outward behaviors. Example: When someone is anxious about germs (obsession), they wash their hands in response (compulsion) etc. However, individuals that suffer with OCD may have mental compulsions that happen internally. Some may count to a certain number or recite words/phrases on repeat until they experience relief from an intrusive thought. Many people often ruminate about the past and re-play scenarios over and over in their head in attempt to gain (a false sense of) mastery over the past, momentarily. Other times, the compulsive behavior can be so small or ordinary it goes unnoticed by the untrained eye. Compulsive behaviors could be as simple as someone nodding their head, doing their laundry, adjusting their body position in a chair, using a certain word in conversation, or checking their space before they leave.
3. OCD is rare in kids: OCD starts at an early age, often before adolescence. Symptoms have been recorded and studied in children as young as 4 years old. OCD is more common in boys up until the age of 10-12, and then evens out in prevalence rate for both genders. OCD symptoms can often peak in these early puberty years, and then again in early adult years (18-25 years). If left untreated, symptoms generally become worse over time as specific treatment (Exposure and Response Prevention Therapy, ERP) is needed to properly target the individual’s OCD symptoms and thoughts, related mood issues, and social/family factors that could be contributing to the pervasiveness of the disorder. Family, parents, or partners are generally involved in the treatment of OCD, as many loved ones unintentionally engage in accommodating/protective behaviors that further fuel OCD symptoms (e.g., allowing your teen to take 2 showers a day because otherwise they appear distressed and cannot focus to do their homework after school).
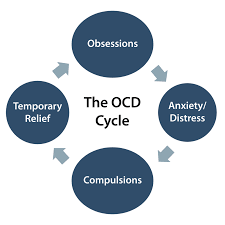
4.“Just tell them everything is fine.” Or “Just tell them NOT to do the compulsion!”: If it was this easy, OCD wouldn’t be listed in the DSM and no one would be upset about having it. One of the hallmark traits about OCD is that intrusive thoughts persist despite ALL evidence. Let’s say someone with OCD knowingly drives over a speedbump in the school parking lot. Their OCD might tell them that although they saw a speedbump, they’ve actually hit a person!! They might tell themselves, “No. I saw that speedbump ahead of me. I go over it every time I drop my son off at school.” Regardless of this evidence, they stop and get out of their car to check behind them. What do they see? Speedbump. Solves it, right? Not really…..They get back in their car and OCD tells them they didn’t check thoroughly enough. They get out one more time to check the spot and surrounding area before they leave. Nothing there, but OCD says differently. They frequently check their rear-view mirror all the way home. Once they park, they check their tires and back bumper to see if there is any damage or evidence of hitting someone. Until they go to pick-up their son at 3pm, they re-play the situation, the sounds, and the feeling of going over that bump throughout their workday, questioning their reality. When an intrusive thought is this anxiety provoking and pervasive, it almost seems impossible to the individual to deny themselves the compulsive behavior that would provide them some temporary relief.

5. People with OCD are perfectionists: OCD stands for Obsessive Compulsive Disorder and consists of two major symptoms: intrusive/unwanted thoughts and compensatory measures in response to these thoughts. Although some symptoms and subtypes of OCD can be related to intrusive thoughts and compulsions around symmetry and orderliness, OCD has a clear distinction from OCPD, Obsessive Compulsive Personality Disorder. OCPD describes characteristics and traits of an individual’s personality that may be a cause for clinical concern. Those who are defined as having an Obsessive Compulsive Personality often have strong preferences for sameness, uniformity, structure, and consistency. They enjoy when things are neat and ordered, are often high-achievers, and place unrealistic expectations of perfection on themselves or others. People with OCPD do NOT suffer from ongoing intrusive thoughts and compulsions. They are often able to tolerate the uncomfortable feelings associated with their preferences (e.g., I really would like these appetizers to be in a straight line, but I don’t want to look weird in front of my guests, so I will just leave them be), and these preferences do not interfere with normal functioning.
6. OCD Is just a phobia or learned fear response: Although there can be some behavioral and conditioning components to OCD, it goes much deeper than just being a learned behavior. When we look at brain scans of those who suffer from OCD, we can see that OCD brains are actually shaped differently than neurotypical brains! Most have a thinner parietal cortex which is the part of the brain involved in response inhibition (aka: thinner parietal cortex = more difficulty controlling impulses). Additionally, brain scans show that many people with OCD are born with less grey matter in their brain, suggesting a genetic and hereditary component to the disorder. Family studies by the National Institute of Mental Health support prevalence rates anywhere from 7-15 % in first-degree relatives. As far as neurotransmitters go (the chemical messengers of our bodies), we can see abnormalities with glutamate and GABA levels in the orbital frontal cortex (OFC) of the brain which is responsible for decision making. Glutamate is an excitatory neurotransmitter and GABA is an inhibitory (calming) neurotransmitter; they depend on each other to function properly (think Ying and Yang). At the risk of getting too sciency on you, you can probably come up with lots of issues that one might experience should there be an imbalance in these two chemicals. Thankfully, there is ongoing and ever-developing research on OCD because we still have a lot to learn and discover.
It is never too early or too late to receive support for OCD. If you or someone you love could benefit from treatment for OCD and its related difficulties, MFS is here to help. Our clinicians are trained in empirically supported methods to help overcome and manage the symptoms of OCD and other anxiety related disorders. Give us a call.


